Iliac Crest Syndrome - A Common Cause of Low Back Pain
 |
| Fig. 1: Pain site at the posterior iliac crest region |
Pain
experienced at the iliac crest is a frequent low back condition
affecting patients seeking help from Sports Medicine Acupuncturists®.
The iliac crest is the top (or ‘crest’) of the ilium, which is
the most superior or upper portion of the pelvic structure. If you
were to place your hands on your hips, they would be resting on the
iliac crest. Pain at the iliac crest, referred to as ‘iliac crest
syndrome,’ is experienced at the posterior (back) portion of the
iliac crest and can be persistent (Fig. 1).
 |
| Fig. 2: Palpation of yaoyan at the superficial and deep vectors |
This
pain is at an acupuncture point called yaoyan which is a
commonly used 'extra point'. Extra points are points which are not on
main acupuncture channels, but have been found to be clinically
important nonetheless. This particular extra point is found at the
attachment site of two important back muscles. Depending on the
depth, these muscles are either the iliocostalis lumborum or the
quadratus lumborum (Fig. 2).
The
iliocostalis lumborum is the more superficial of the two of these
muscles. It is one of three muscles which are part of a group called
the erector spinae (Fig 3 left image). This is the group of muscles that span the back
from the hip through the neck and run parallel to the spine. The
iliocostalis lumborum is the ‘lumbar’ or low back portion of this
group; it runs from the top of the iliac crest (the ‘ilio’ part
of the name) to the ribs (the ‘costo’ part of the name). This
muscle then continues upward (but it is then called the iliocostalis
thoracic and iliocostalis cervicis) and is the most lateral of the
three muscles of the erector spinae. The iliocostalis functions with
the other muscles of this group to perform extension of the torso,
which is the motion involved in bending backward. However, since this
muscle is a bit more lateral than the others in the group, it is also
involved in side bending motion. In this case, only one side is
primarily involved–the
right muscle in right side bending and the left in left side bending.
The
quadratus lumborum is a deeper muscle underneath the iliocostalis (Fig. 3 right image). It
runs from the iliac crest and has attachments on the lumbar (low
back) vertebrae, and ends at the 12th (lowest) rib in the
back. This muscle laterally flexes the trunk. It does this by
shortening the space between the top of the hip and the 12th
rib. This would either pull the rib towards the hip (sidebending on
that side) or pull the hip towards the rib (elevating or hiking the
hip up on that side).
Both
of these muscles have attachments on the iliac crest and both can
become pain-producing sites. In both cases, these muscles would be in
a shortened position when the hip is hiked on the side of pain. This
is frequently what is seen with iliac crest pain.
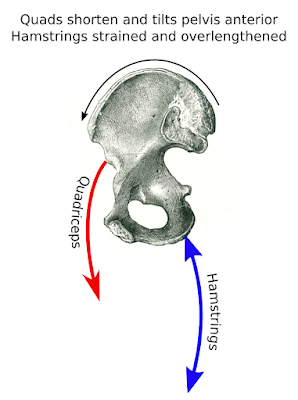
When
the hip is elevated on one side, as is often the case with iliac
crest syndrome, it is not simply the muscles discussed which are
involved. Other muscles whose job it is to stabilize the hip and
prevent it from elevating are also part of the overall picture. The
gluteus medius and minimus are the primary muscles which do this, and
these muscles have a propensity to become inhibited and fail in their
stabilization roll.
When treating iliac crest syndrome, it is important to address all of
the muscles involved in the imbalance. This includes both the
shortened and overactive muscles such as the iliocostalis and
quadratus lumborum, along with the inhibited and overlengthened
muscles such as the gluteals. Acupuncture and manual therapy are
powerful treatment options to correct these imbalances, and
corrective exercises performed by the patient can solidify treatment
at continue to return function.